Fig.28. Sphygmomanometer: with spring manometer, with mercurial manometer
The nurse puts down the readings of manometer into the temperature form as red columns corresponding to the AP scale.
AP can be also measured by the oscillographic method. Besides measuring the AP it also allows to assess the state of the vascular wall, vascular tone, blood velocity. Under computer processing the following values are calculated as well: ventricular ejection (VE), circulation rate (CR), general peripheral vascular resistance (GPVR) and their accordance.
- An adult’s normal SAP is between 100 and 139 Mmhg, DAP – between 60 and 89 Mmhg.
AP is considered to be high from 140/90 Mmhg and more (arterial hypertension or hyperpiesis) and to be low from 100/60 Mmhg and less (arterial hypotension). A sudden rise of AP is called hypertensive crisis. Besides the sudden pressure rise it also declares itself in severe headache (cephalea), dizziness, nausea and vomiting.
Classification of AP levels of adults over 18 year old (in accordance with recommendations of WHO, World Society on Studying Arterial Hypertension, JNC VI (Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure) and Russian national recommendations on arterial hypertension, 2001) is in the following table:
Classification of AP levels
| Categories of AP | SAP, | DAP |
| Mmhg | Mmhg | |
| Categories of normal AP | ||
| Optimal | <120 | <80 |
| Normal | <130 | <85 |
| High normal | 130-139 | 85-89 |
| Categories of high AP | ||
| Arterial hypertension | ||
| 1 degree | 140-159 | 90—99 |
| 2 degree | 160-179 | 100-109 |
| 3 degree | > 180 | > 110 |
| Isolated systolic hypertension | > 140 | <90 |
If the SAP and DAP values appear in different categories, the higher one is chosen.
When attending a patient with arterial hypertension it is necessary to pay rapt attention that patients adhere to all the requirements of medial protective regimen because negative emotions, neuropsychic strain, bad sleep can aggravate clinical course.
Hypertensive crisis requires immediate doctor’s intervention and introduction of antihypertensive drugs since it may be complicated by stroke (cerebral crisis) and coronary circulation disorder (myocardial infarction). Before the doctor’s arrival it is necessary to provide absolute rest, inflow of fresh air; hot foot bath and warm hand bath (t° of water 37-40°C) can be useful.
Even absolutely healthy people, especially asthenics, can have arterial hypotension but it can also be a symptom of serious diseases accompanied by low ventricular ejection, vascular tone and reduction of blood volume (myocardial infarction, haemorrhages, shock, collapse). A patient with acute arterial hypotension is to be put to bed, the foot end of the bed should be lifted a little to improve blood flow to the brain, it is necessary to introduce the drugs prescribed by the doctor.
Common symptoms of disease of cardio-vascular system, observing and attending patients
Pains in heart region
When assessing pain complaints in heart region it is necessary to bear in mind that it is not always that they are caused by diseases of cardio-vascular system. Pains can develop as a result of diseases of pleura (dry pleuritis), vertebral column and intercostal nerves (intervertebral osteochondrosis, intercostal neuralgia), of myositis, hiatal hernia, etc.
Pains in the thorax concerned with pathology of blood circulation system can be caused by pathology of pericardium, aorta, neuroticism. But the most important for diagnosing, further tactics and prognosis is the development of heart stroke.
Heart stroke develops when coronary arteries constrict due to their atherosclerotic damage, vasospasm may accompany it. During heart stroke there is an imbalance between the need of myocardium for oxygen and the potential of coronary blood flow, which leads to ischemia, hypoxia. Metabolism is broken and under-oxidated metabolic products stimulate the sensory receptors in myocardium causing pain.
In typical cases heart stroke is caused by physical or emotional activity. Retrosternal pains of pressing, burning or gripping character develop, accompanied by apprehension of death, shooting up to left shoulder, arm, left half of the neck, lower jaw, lasting from one to ten minutes and passing off at rest by itself in 1-3 minutes after taking a pill of nitroglycerine under the tongue.
A patient with heart stroke can be helped by: providing absolute rest, taking nitroglycerine under the tongue and less often – by applying mustard plaster on the heart region. A very severe disease that usually complicates the heart stroke, which is not controlled protractedly, is myocardial infarction that is based on necrosis (mortification) of a part of cardiac muscle.
The most widely-spread, the so-called typical (algesic, anginous) myocardial infraction is characterized by the development of pain behind sternum – extremely severe pain that can be controlled neither by rest, nor by taking nitroglycerine, that last more than 30 minutes (up to several hours). Such pain is accompanied by apprehension, asthma, sudden asthenia, pressure fall, etc. Such patients need urgent hospitalization (during the first hours of the disease) to a special care ward equipped with all the apparatuses necessary for monitoring (automatic constant observation) the patients’ state and carrying out resuscitation procedures. In the first days patients are prescribed absolute bed rest; during this period control over the state of bed, the patient’s clothes and bed linen, accomplishment of all hygienic procedures, nutrition of patient, giving the bedpan and urinal is required.
Dyspnea, paroxysmal dyspnea and pulmonary edema
When accompanying diseases of cardio-vascular system, dyspnea is one of the signs of circulatory collapse that is based on depression of contractile function of myocardium and declares itself by bradyhemarrhea in greater and lesser circulation and by retention of liquid in the organism. In cases of cardiac dyspnea blood is accumulated in the lesser circulation and the patient has an oppressive feeling of shortness of breath: at first during physical activity and excitement but with progression in rest as well.
Asthma (paroxysmal dyspnea) in cases of circulatory collapse is a sudden, severe attack of asthma accompanied by stentorious breathing, it usually develops at night (because of hypersthenia of nervus vagus which causes constriction of coronary vessels). The patient tries to sit forcedly (orthopnea). The attack of paroxysmal dyspnea develops when there is a sudden reduction of contractility of heart muscle due to its necrosis (infraction), inflammation (severe myocarditis) or overstrain (hypertensive crisis, inadequate physical activity).
The most severe display of circulatory collapse is pulmonary edema, when the liquid component of blood perspires through the vessel walls and is accumulated in alveoles. In this case bubbling breathing and discharge of pink albuminoid sputum is added to the above-mentioned symptoms of paroxysmal dyspnea.
In cases of dyspnea the patient can be helped by: absolute rest, being in a sitting or semi-sitting position (orthopnea), removing hampering clothes, a flow of fresh air, taking nitroglycerine (if there are no contra-indications) or an antihypertensive on the doctor’s prescription if the pressure is high.
Paroxysmal dyspnea and pulmonary edema require the following relief measures:
- first of all a doctor must be sent for;
- to place the patient in a sitting position (orthopnea);
- to give nitroglycerine if the patient’s systolic pressure is not lower than 100 Mmhg;
- to start oxygen therapy through the mask or nose catheter with an anti-foaming agent; usually 96% ethyl alcohol is used as the anti-foaming agent, which is poured into the dosimeter or a special humidifier; oxygen goes through the latter;
- it is necessary to suck out (aspirate) albuminoid sputum with an electric suction machine;
- after placing the patient in a sitting position tourniquets are applied on the legs to stagnate the blood in greater circulation and hold back its coming to the lungs.
To do this tourniquets or a rubber tube or a tonometer pressure cuff is applied on both legs 15 cm lower than the inguinal fold; only veins should be constricted, i.e. the arterial pulse lower the tourniquet must be preserved and the limb must become cyanochroic; time of tourniquet application is 15-20 minutes;
- venous tourniquets may be applied on arms too. The tourniquets must be removed in series (first from one hand, in some time from another hand, etc.) slowly;
- it is possible to use phlebotomy to remove some of the circulating liquid from blood flow and to relieve the lesser circulation;
- hot foot baths are used;
- on the doctor’s prescription drugs, diuretics, cardiac glycoside, etc. are introduced intravenously.
Edemas
In cases of circulatory collapse edemas are the result of bradyhemarrhea in the greater circulation and of retention of liquid in the organism. Cardiac edemas are most often localized in legs, if the patient walks, or in the area of sacrum, lumbus, scapulas, if the patient lies. Skin in the area of edema becomes smooth, shiny, tight; when pushed on, there remains a small pit that does not get smoothed out for a long time. In neglected cases of circulatory collapse liquid (transudate) can be accumulated in serous sacs – abdominal cavity (ascites), pleural cavity (hydrothorax), pericardial cavity (hydropericardium); edema of the whole body is called anasarca.
When observing and attending patients with circulatory collapse it is necessary to remember that edemas can be obscure at early stages of the disease. If that's the case, retention of liquid in the organism can declare itself by a quick increase of body weight and decrease of diuresis. That is why it is very important to daily control water balance of such patients, i.e. to compare the amount of drunk and parenterally introduced liquid with the amount of urine discharged in the last 24 hours (daily urine). Daily urine must be 1,5-2 l (70-80% of volume of all liquids consumed in the last 24 hours). If less urine than 70-80% of volume of all liquids consumed in the last 24 hours is discharged, negative diuresis is verified, i.e. some of the liquid is retained in the organism. If the amount of urine exceeds the amount of consumed liquid, it is ecuresis. Ecuresis also takes place when edemas are coming off, when taking diuretics.
Water balance can also be controlled by weighing the patient: increase of body weight is evidence of retention of liquid. It is necessary to remember that patients confined to bed and taking diuretics must be provided with urinals, bed-pans.
When a large amount of liquid is accumulated in the abdominal cavity, abdominal paracentesis is carried out for diagnostic and medicinal purpose. When puncturing, it is necessary to be careful, since removal of large amount of liquid at one stroke may cause collapse.
Patients with chronic circulatory collapse confined to bed often develop nutritional changes in the area of edema – area of sacrum, lumbus, scapulas, that is why there is a good likelihood that bedsores appear.
Syncope
Syncope – is a temporary loss of consciousness caused by abrupt cerebral circulatory insufficiency. Usually syncope results from strong neuropsychic impact (fright, acute pain, sight of blood), from being in a stuffy room, from bad defatigation. The patient feels giddy, sonitus, blackout and looses consciousness. Paleness of skin and visible mucosa, extremities coldness, cold clammy sweat, sudden fall of AP, small, thready pulse is marked in such cases. As a rule, syncope lasts 20-30 seconds, after that the patient regains consciousness.
In cases of syncope the patient can be helped by: being in a recumbent position with the legs lifted a little (to promote blood flow to the head), removing hampering clothes, providing a flow of fresh air. One may rub the patient’s temporal fossae and chest, sprinkle some cold water on the face, put a cotton-wool ball soaked in liquid ammonia to the nose (to activate the inspiratory center)
Collapse
Collapse is a clinical implication of vasogenic shock with sudden fall of AP and peripheral circulatory failure, it is noted in cases of acute blood loss, myocardial infarction, in orthostasis, dehydration caused by repeated vomiting and diarrhea. Clinical implications are similar to those of syncope but collapse is not always accompanied by loss of consciousness, the patient can be only retarded, apathetic, the pupils become mydriatic.
In cases of collapse the patient can be helped by: being in a recumbent position with the head down, bleeding control, warming. If needed, parenteral adjustment of circulating blood volume is carried out on doctor's orders through infusion of whole blood or blood substitutes; introduction of drugs increasing vascular tone (Cordiaminum, Sulfocamphocain, Mesaton, etc.) is also possible.
Observing and attending patients with diseases of digestion organs
Anatomic-physiological peculiarities of gastrointestinal tract
The source of nutrients necessary for normal functioning of the human body is food. Due to it energy consumption is met and plastic processes are realized. Proteins, carbohydrates, mineral salts, vitamins get into the organism with food. However the majority of these substances cannot penetrate through cell membranes and be soaked in blood in the state in which they are in food. They should be divided into more simple compounds and this is what is carried out in the gastrointestinal tract as a result of the digestion process.
Digestive system carries out the following functions.
Movement (motor) function consists in moving the food in the gullet, stomach, small and large intestine and in discharging undigested remains from the organism.
Secretory function is production of digestive juices by gland cells: saliva, gastric juice, pancreatin, intestinal juice, bile. Juices contain enzymes that split proteins, fats, carbohydrates into more simple chemical compounds – amino acids, glycerin, fatty acids and monosaccharides. Mineral salts, vitamins, water join blood in the same form, they are not split.
Excretory function is carried out by removing metabolic products from the organism – cholechromes, urea, ammonia, salts of heavy metals, medicinal substances and, at last, absorbing function – absorbtion by the mucous coat of stomach and, especially, by the mucous coat of intestines.
Main symptoms of digestion organs diseases
Diseases of digestion organs are studied in the section of internal medicine that is called gastroenterology. Pains are to be attributed to the main symptoms of digestion organs diseases. The following pains are distinguished: peritonealgia (involvement of peritoneum, which covers digestion organs, into disease process), and visceral (when the motor function of digestive tract is disturbed – spasm, stretching, atony).
Peritonealgia is usually constant, acute, lancinating, increasing with body movements, accompanied by rigidity of abdominal muscles.
Visceral pains are colicky, dull, extended. Pains in the stomach are not always the symptom of digestion organs diseases. The decision about carrying out any medical actions in connection with pains in the stomach must be made by the doctor.
Pains at gastroenterologic diseases can be accompanied also by various dyspeptic disorders: nausea, eructation (emission of gases or food bits from the stomach cavity into the oral cavity), vomiting, orexia disorder, constipation, diarrhea, tympania (drum belly).
Vomiting – is a dyspeptic disorder, the act of involuntary discard of the stomach or intestine contents through the gullet and pharynx into the mouth cavity, nasal passages.
Attendance in cases of vomiting
During vomiting the patient is made sit down or lie sideways, the head is bent down, a basin is placed on the floor and a dish or a towel is brought to the angle of mouth. After vomiting the patient is given some water to rinse the mouth (the nurse clears the oral cavity of serious patients with a cotton ball wetted in water or weak solution of sodium hydrogencarbonate, potassium permanganate), is put to bed, covered with a blanket. If there is a touch of blood in vomiting matters, the patient must not drink, take drugs, eat; an ice-bag is put on the anticardium, pulse (frequency, strength) is taken, arterial pressure is measured, the doctor is sent for.
Vomiting matters are collected at each vomiting for the following purposes: to measure their amount and determine their composition with subsequent laboratory examination. A glass container with a wide neck, with a capacity of up to 2 litres, with graduation lines on the side and with a closable lid, is the most convenient thing for collecting them. Vomiting matters are kept until the doctor comes and decides whether to send them for laboratory examination or not.
Gastric lavage
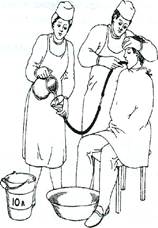
The procedure is carried out for medical and diagnostic purposes. The device for the lavage consists of a glass funnel of 0,5-1 l in volume, connected with a thick gastric tube with a diameter of 1 cm, 1,5 m long. A clean tube is boiled beforehand and put in cold boiled water for cooling before the procedure. The lavage is carried out with water of 20 °-30 оС, total amount - 5-10 litres( Fig.29).
Diagnostic lavage is carried out if there is a suspicion of stomach cancer (tumour – atypical cells can be found in lavage water). Domiciliary gastric lavage consists in giving the patient 4-8 glasses of water to drink, and then he is vomited by pressing on root of tongue or by irritating the back of the throat. This procedure is repeated several times.

А б
Fig. 29.Sequence of placing (a), gastric lavage the funnel when performing gastric lavage (b).
Preparation of the patient for roentgen examination of stomach and small intestine
Roentgen methods (rontgenoscopy – transmission and direct observation, rontgenography – shots and analysis of prints) allow to study the pathology of gastrointestinal tract most fully. With the help of this method it is possible to find out the form, position, relief of the mucous coat of stomach and duodenum. Roentgen examination of stomach and intestines is carried out using radiopaque substance: barium suspension (100 gr in 100 ml of boiled water). The suspension is ingested just before the examination.
Preparation of the patient for roentgen research aims at emptying the contents of the stomach and intestines to the maximum (food debris, liquid, gases). During three days prior to examination the patient must not eat products causing abundant generation of gases (rye-bread, milk, potatos, etc.). To reduce gas generation the patient is given a glass of camomile tea (1 table- spoon for 1 glass of water) a day or 2 pills of activated charcoal 3-4 times a day during 2-3 days. In the evening before the examination and in the morning of examination the patient is given a cleansing enema. It is better to carry out roentgen examination of stomach in the morning on an empty stomach.
Fractional examination of gastric material
This method of examination is carried out by introduction of a tube for taking the contents of the stomach for the purpose of calculating the amount and composition of gastric juice, of determining the state of secretory and motor functions of the stomach, of revealing other pathological admixtures in contents( Fig.30).
To extract the contents from the stomach a thin gastric tube 70-75 cm long, with outer diameter of 4-5 mm, inside diameter of 2-3 mm, with two oval openings on the closed end that is introduced into the stomach lumen, and with three marks (the first mark – the end of the tube is in the forestomach, the second – in the area of the stomach sinus, the third – at the stomach exit), is used. For full extraction of gastric juice the end of the tube must be in the area of stomach sinus (the second mark). After introducing the tube (method of introduction is the same, as for gastric lavage) a syringe is attached to its external end and all gastric material is extracted – this is a portion on an empty stomach. Then during one hour a basal portion is received: the gastric material is divided into 4 portions received within each 15 minutes.
After the extraction of the basal portion an irritant is introduced to get a stimulated portion of gastric juice. To do this, various irritants are used: oral and parenteral.
Oral test-breakfasts: 300 ml of 7% cabbage broth (by Leporsky), grain broth - 35 gr of white bread in 400 ml of tea (by Boas-Ewald), 200 ml of meat broth (by Zimnitsky). When oral irritant is used, the remains of the test-breakfast is pumped out in 25 minutes, and then 4 portions of stimulated secretion are received each 15 minutes within one hour.
Parenteral test-breakfasts: histamine and pentagastric secretin. Histamine dihydrochloride is introduced hypodermically in a doze of 0,008 mg per kilo of the patient’s body weight or 0,1 ml of 0,1 % of solution per 10 kg of the patient’s body weight. It is possible to use pentagastric secretin instead of histamine in a doze of 6 mkg per kilo of the patient’s body weight. When using parenteral irritant during the next hour every 15 minutes, 4 portions of gastric material are drawn up – this is the stimulated portion. At this point the procedure is finished – the tube is taken out of the stomach.

